Research to Prevent Blindness (RPB) is celebrating 30 years of its highly impactful Career Development Awards, which jump-start research early in the careers of outstanding scientists.
Sixteen UCSF vision scientists have received Career Development Awards over the years, advancing new knowledge, insights, and solutions — building blocks in the future of vision. UCSF vision research continues to benefit from these and other RPB awards, including three this year.
 Nurturing Novel Approaches
Nurturing Novel Approaches
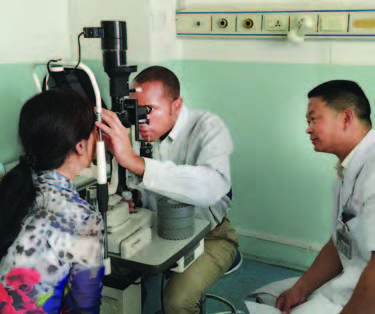
Thuy Doan, MD, PhD, applied her 2016 RPB Career Development Award to help launch pioneering genomic studies of the ocular micro-environment (biome) in search of pathogens underlying uveitis inflammations.
Dr. Doan’s international work at the Proctor Foundation involves investigation of the intestinal microbiome for an antibiotics study of 190,000 children in sub-Saharan Africa. Dr. Doan is lead author of a new Proctor publication in Nature Medicine,* which posits that reductions in two diarrhea-related bacteria may be a factor in higher child survival rates.
“Those of us who study… child survival in sub-Saharan Africa haven’t seen well-done trials showing such a striking mortality benefit in a really long time, so it’s very exciting,” says Patricia Pavlinac, MD, a University of Washington epidemiologist.

Preventing AMD
Retinal cell biologist Aparna Lakkaraju, PhD, won RPB’s 2019 Catalyst Award for Innovative Approaches to Age-Related Macular Degeneration (AMD). Her team uses innovative microscopy, genome editing, and stem cell technologies to pinpoint genetic and cellular mechanisms responsible for initiating AMD, and identify promising therapies to target the earliest disease stages to preserve central vision. The research builds on earlier successes made possible by her Career Development Award in 2010.
Understanding Epidemics
RPB collaborates with the American Academy of Ophthalmology to grant awards for big data research. Michael Deiner, PhD; Thomas Lietman, MD; and Travis Porco, PhD, won this 2019 award to use the exceptional IRIS Registry to study infectious eye epidemics in the United States.
Strategic Flexibility
The Department of Ophthalmology was awarded an RPB unrestricted grant this year as well. The five-year grant extends decades of institutional support from the foundation. “We’re extremely grateful,” says Department Chair Stephen D. McLeod, MD. “These awards allow us to build high potential research from the ground up.”
*T Doan, A Hinterwirth, L Worden, AM Arzika, R Maliki, A Abdou, S Kane, L Zhong, SL Cummings, S Sakar, C Chen, C Cook, E Lebas, ED Chow, I Nachamkin, TC Porco, JD Keenan, TM Lietman. “Gut microbiome alteration in MORDOR I: a community randomized trial of mass azithromycin distribution.” Nature Medicine. 2019 Aug 12.