K12 Program Mentors

The mentors available to UCSF-Proctor Clinician Vision K12 Scholars have been chosen from a wide range of research disciplines to represent Track 1 (epidemiology/RCTs/global health), Track 2 (basic and translational discovery sciences), and Track 3 (bioengineering & innovation). Track 2 includes Mentors focused on basic and translational vision discovery sciences across three themes (ocular genetics & therapeutics; visual system injury, plasticity & regeneration; and neurodegeneration). A major strength of our program is the close collaboration among Department of Ophthalmology and Proctor faculty and between Ophthalmology/Proctor faculty with other UCSF faculty. Each of the proposed Mentors is a recognized and well-funded independent investigator with a successful track record of mentoring and providing research training and career development to graduate students, residents, clinical and postdoctoral fellows, and junior faculty. Most of the Mentors currently collaborate with one another and other UCSF faculty.

Efficient RCTs. RCTs in the US funded by the NIH can easily cost $10,000 to $100,000/case. With so many questions unanswered, and so many new questions being posed every year, more efficient trial design could be a way to make up for limited resources. Proctor-UCSF is currently running several large simple trials, cluster-randomized trials, and adaptive trials. We capture data from some of the poorest areas on earth and upload directly to the cloud to streamline our Data Coordinating Center. We have taken advantage of international collaborations to increase efficiency of enrollment. Our goal is to expose Scholars to a number of novel mechanisms to make RCTs more efficient. We encourage them not to put their effort into lobbying for $15 million to do a study, but instead to figure out how to answer the question rigorously at a fraction of what it would cost others.
A note about RCTs: It is unlikely given the timeline and budget that a Scholar would initiate their own RCT as their K project. However, if/when scholars decide they would like to answer a secondary question from an existing trial or gain research experience by participating in an ongoing trial, we would contact the NEI program administrator to get permission. We would work with the Scholar to provide justification for how the proposed study would (a) include administrative, data coordinating, enrollment and laboratory/testing centers, appropriate for the trial proposed; (b) adequately address the capability and ability to conduct the ancillary study at the proposed site(s) or centers; (c) if applicable, appropriate plans to add or drop enrollment centers, as needed; (d) if international site(s) is/are proposed, adequately address the complexity of executing the clinical trial; (e) if multi-sites/centers, demonstrate of the ability of the individual site or center to: (1) enroll the proposed numbers; (2) adhere to the protocol; (3) collect and transmit data in an accurate and timely fashion; and, (4) operate within the proposed organizational structure.
 Global Health. A number of research questions can better be addressed through international collaborations. 30 years ago, trachoma and onchocerciasis were two of the leading causes of blindness worldwide. Now the opportunity exists not just control, but to eradicate these diseases. We anticipate that community-randomized trials will be required to accomplish this goal. While trachoma was eliminated from the US in the 1970s and onchocerciases was never a public health problem in the US, the NEI has recognized that eradication of these two diseases is part of their strategic plan. The uveitis found in Ebola survivors can be studied in Liberia and Democratic Republic of Congo, but not in the US. Other diseases, such as fungal keratitis, are present in the US, but have a far higher incidence in tropical areas of the world such as South India. Studies which benefit both US and Indian patients can be done far more easily abroad. Diseases that are relatively common in the US such as uveitis can be studied with multi-country collaborations. This can decrease enrollment time and cost, and increase generalizability, as well as take advantage of some of the clinical expertise worldwide. In many ways, other medical systems outside of the US are better prepared to enroll and monitor trial patients, and international collaborations can take advantage of this.
Global Health. A number of research questions can better be addressed through international collaborations. 30 years ago, trachoma and onchocerciasis were two of the leading causes of blindness worldwide. Now the opportunity exists not just control, but to eradicate these diseases. We anticipate that community-randomized trials will be required to accomplish this goal. While trachoma was eliminated from the US in the 1970s and onchocerciases was never a public health problem in the US, the NEI has recognized that eradication of these two diseases is part of their strategic plan. The uveitis found in Ebola survivors can be studied in Liberia and Democratic Republic of Congo, but not in the US. Other diseases, such as fungal keratitis, are present in the US, but have a far higher incidence in tropical areas of the world such as South India. Studies which benefit both US and Indian patients can be done far more easily abroad. Diseases that are relatively common in the US such as uveitis can be studied with multi-country collaborations. This can decrease enrollment time and cost, and increase generalizability, as well as take advantage of some of the clinical expertise worldwide. In many ways, other medical systems outside of the US are better prepared to enroll and monitor trial patients, and international collaborations can take advantage of this.
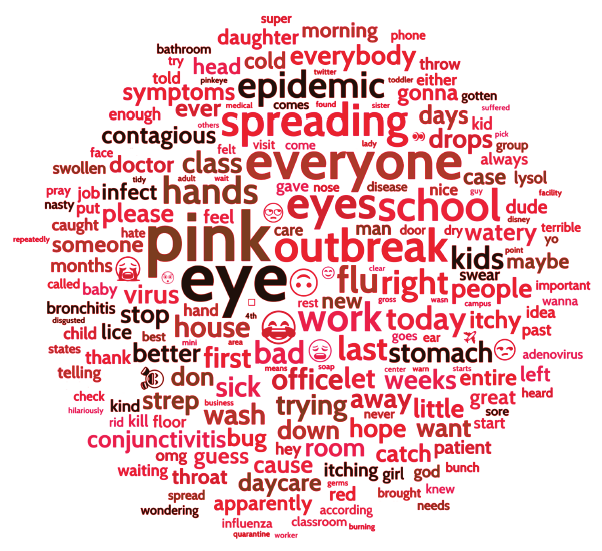
Computational health sciences and big data. Technological innovations have converged to create big data. UCSF’s vision scientists now routinely use massive, diverse, and searchable databases to help answer vital research questions more quickly and clearly than ever. The Proctor Foundation and the Department of Ophthalmology are jointly establishing a big data group, led by data scientist Michael Deiner, PhD, and including a dozen faculty with ongoing funded projects including three NEI big data R01s and three OPTUM awards. Projects include detecting pink eye epidemics worldwide from social media and forecasting trachoma eradication from the world’s collected surveys. Corneal ulcers, herpes simplex, and herpes zoster have been studied in the Kaiser Hawaii and Northern California databases, and now the effect of the new vaccine on Zoster Ophthalmicus is being tracked with OPTUM. The IRIS database is being used to test the hypothesis that metformin may affect the course of AMD. Next generation sequencing provides by far our largest databases–a number of NEI-funded projects include deciphering the genetics of glaucoma and discovering novel ocular pathogens.
Track 1 faculty include:
Nisha Acharya, MD, MS (Advisory Committee) is the Elizabeth C. Proctor Distinguished Professor at the F.I. Proctor Foundation and Departments of Ophthalmology, Epidemiology and Biostatistics at UCSF and the Director of the Uveitis and Ocular Inflammatory Disease Service. Dr. Acharya is a clinician-scientist with fellowship training in cornea and uveitis, with a clinical focus of ocular inflammatory diseases and uveitis. Her research focuses on clinical trials and epidemiological studies in ocular inflammation. She was co-PI of the U10 Mycotic Ulcer Treatment Trial, and is currently PI of the NEI-funded U10 grant First-line Antimetabolites for Steroid-Sparing Treatment (FAST) Uveitis Trial, a multicenter trial comparing methotrexate to mycophenolate for the treatment of non-infectious intermediate, posterior, and panuveitis. She is the PI of the U10 ADJUST (Adalimumab in juvenile idiopathic arthritis-associated uveitis). She is also protocol co-chair of a macular edema trial through the Multicenter Uveitis Steroid Treatment Trial group. Dr Acharya’s research group is experienced in working with large electronic medical record datasets. She was the PI of the Pacific Ocular Inflammation Study, which was a collaboration with Kaiser Permanente Hawaii that focused on the epidemiology of ocular inflammatory diseases. She also runs an R01 grant studying the effectiveness of the herpes zoster vaccine for herpes zoster ophthalmicus using multiple large data sources. Dr. Acharya mentors several medical students performing year-long research projects, residents, clinical fellows, and junior faculty (including K23 awardee Thuy Doan, MD, PhD). Scholars interested in RCTs and epidemiological studies addressing uveitis may select Dr. Acharya as a Mentor.
Jeremy Keenan MD MPH, H. Bruce Ostler Professor of Ophthalmology and the Director of International Programs at the Proctor Foundation, is an epidemiologist and ophthalmologist with clinical specialties of cornea and uveitis. His research focuses on strategies to reduce the global burden of blindness, with an emphasis on developing countries. Dr. Keenan is currently the PI of two UG1 grants from the NEI: SWIFT (Sanitation, Water, and Instruction in Face-washing for Trachoma), a cluster-randomized trial that seeks to determine whether improvements in water, sanitation, and hygiene are effective for infectious trachoma in Africa, and VIEW II (Village-integrated Eye Worker Trial II), a cluster-randomized trial that seeks to determine the effectiveness of community-based screening for glaucoma, diabetic retinopathy, and macular degeneration in Nepal. Dr. Keenan is also a co-investigator on several trials funded by the Gates Foundation to determine the effectiveness of mass azithromycin distributions for childhood mortality. In addition, he has strong ties to Aravind Eye Hospital in South India, where he is conducting a pilot trial comparing different treatments for acanthamoeba keratitis, and with Chiang Mai University in Thailand, where he has performed diagnostic accuracy studies for cytomegalovirus retinitis, glaucoma, and diabetic retinopathy. He has been the primary mentor to six medical students who have done a research year between third and fourth year of medical school and has also served as a mentor to a doctoral candidate in epidemiology, who completed her dissertation work alongside the SWIFT trial in Ethiopia. Dr. Keenan may be a Mentor to those Scholars interested in international RCTs addressing major public health problems.
Thomas Lietman, MD (Co-PI/Co-PD) is the Ruth Lee and Phillips Thygeson Distinguished Professor in the Department of Ophthalmology and Department of Epidemiology & Biostatistics, and the Director of the Francis I. Proctor Foundation. His research group has considerable experience with individual and community-randomized trials of trachoma, childhood mortality, and corneal ulcer treatment and prevention. He has served as the PI on a number of NIH-funded clinical trials: the Steroids for Corneal Ulcer Trial (SCUT I), the two Mycotic Ulcer Treatment Trials (MUTT I and MUTT II, with Dr. Acharya), the two Trachoma Amelioration in Northern Amhara studies (TANA and TIRET), and the Village Integrated Eye Worker trial (VIEW, in Nepal). He is multiple PI (with Dr. Oldenburg) on the Ethiopian trachoma trial KETFO and (with Dr. Rose-Nussbaumer) on the ongoing SCUT II corneal ulcer trial. In addition, he was the overall PI on the Bill and Melinda Gates Foundation (BMGF)-funded MORDOR I study (with Drs. Oldenburg, Keenan, and Doan) and for the MORDOR II studies (Niger and Burkina Faso), as well as the AVENIR planning grant (Niger). He ran the Niger arm of the BMGF-funded PRET trachoma study (PI Dr. Sheila West, Johns Hopkins), and has worked on the BMGF-funded Neglected Tropical Disease modeling consortium (PI Deirdre Hollingsworth, Oxford University). Recently, he has explored big data for infectious disease, including two NEI projects: the Digital Disease Detection grant locates pink eye epidemics in the US and internationally from web searches, electronic medical records, and social media, and the Forecasting Trachoma grant (multiple PI with Dr. Porco) which uses several large databases to determine if and when trachoma will be controlled worldwide. His group has predicted, monitored, and assessed the clinical implications of antibiotic resistance in NIAID, NEI, and BMGF grants (including PREDICTING RESISTANCE, SCUT, MUTT, TANA, MORDOR). He has had the opportunity to be the primary mentor on five K23 awards, two of which are still ongoing. Scholars interested in RCTs related to infectious diseases and childhood mortality, as well as big data, may identify Dr. Lietman as a Mentor.
Catherine Oldenburg, ScD, MPH, Assistant Professor of Ophthalmology and Epidemiology & Biostatistics, is an infectious disease epidemiologist who uses randomized controlled trial designs to evaluate antibiotic-based interventions to prevent childhood morbidity and mortality in sub-Saharan Africa. Her expertise includes infectious disease epidemiology, causal inference, and global health. Current projects include evaluation of core-group based targeting strategies for trachoma elimination in Ethiopia and administration of azithromycin to young infants and neonates for the prevention of child mortality in Burkina Faso. Dr. Oldenburg serves as a mentor on the Resident Research Committee in the Department of Ophthalmology (approximately ten resident projects per year). She also serves as a research mentor for epidemiology graduate students, medical students, and undergraduate students interested in clinical research and public health. Dr. Oldenburg may be identified as Mentor for those Scholars interested in RCT design, infectious disease epidemiology, and global health.
Travis Porco, PhD, MPH, Professor of Epidemiology & Biostatistics and Ophthalmology, is a mathematical epidemiologist and biostatistician who has contributed to projects involving trachoma, Ebola virus disease, measles, and other communicable diseases. He has been the biostatistician for numerous NEI RCTs, including MUTT I and II, SCUT II, TANA I and II, SWIFT, FAST, ADJUST, and KETFO, and multiple BMGF trials including PRET-Niger, MORDOR I and II, NAITRE, CHAT, and CHATON. He is multiple PI on the NEI Trachoma Forecasting grant, and PI on an NIH EBOLA forecasting grant. Dr. Porco has considerable experience in mentoring residents and research fellows in study design, having a hand in most of the resident and fellow research projects over the last ten years. Scholars interested in mathematical modeling and biostatistics may identify Dr. Porco as a Mentor.
The Department is proud of the range of basic and translational vision science research that is currently supported from basic cellular and molecular processes that are fundamental to the physiology of the visual system through laboratory-based translational work. We have a particular focus on regenerative medicine cutting across ophthalmological disciplines, and our current team reflects specific expertise in three thematic areas: ocular genetics & therapeutics, visual system injury, plasticity, and regeneration, and neurodegeneration. In addition, we have a Core grant for vision research (P30) that supports investigators via core modules.
Faculty Mentors on this Track include:
Matilda Chan, MD, PhD, Associate Professor of Ophthalmology, is a cornea clinician-scientist interested in understanding the molecular mechanisms underlying corneal injury, inflammation, and repair. Dr. Chan’s R01 is focused on the role of matrix metalloproteinases (MMPs) in modulating various aspects of corneal repair after injury including inflammation, neovascularization, and fibrosis. She is also studying the epigenetic and genetic alterations underlying Fuch’s endothelial cell dystrophy (FECD), specifically the role of DNA methylation as a mechanism for silencing genes during disease pathogenesis. In collaboration with Jason Gestwicki (UCSF), her group is using high throughput screening to identify compounds for the treatment of FECD. Dr. Chan has mentored undergraduates, medical students, postdoctoral fellows, residents, and clinical fellows. The Chan lab would provide opportunities for Scholars interested in the role of extracellular matrix in ocular disease, epigenetics, and translational vision science.
Bruce Conklin, MD, Professor of Medicine, is a Gladstone Research Institute senior investigator who leads a well-funded NIH-supported lab that focuses on genome engineering to cure human genetic diseases. In collaboration with Drs. Jacque Duncan and Tony Moore, the group is developing an in vivo gene editing approach to inactivate the disease allele in the retina for autosomal dominant vitelliform degeneration. Using this approach, normal bestrophin function can be restored. Dr. Conklin has mentored many graduate students and postdoctoral fellows in the lab, and now serves as Associate Director of the Gladstone’s California Institute for Regenerative Medicine (CIRM)-funded training program. Scholars interested in the use of state-of-the-art genome editing strategies in ocular genetics and therapeutics may identify Dr. Conklin as a Mentor.
Xin Duan, PhD, Assistant Professor of Ophthalmology, is a developmental neurobiologist and expert in retinal circuitry. He is interested in the molecular and cellular basis of neural circuit wiring and rewiring, with the goal of reconstructing neural circuits and restoring normal function in the setting of neuronal injury. Specifically, the Duan lab is focused on identifying the determinants of synaptic specificity and the regenerative abilities of specific retinal neuron subtypes. Recently, Dr. Duan was awarded a Catalyst for a Cure grant to restore vision in glaucoma via axonal regeneration. He has successfully mentored many students, and currently has several graduate students and postdoctoral fellows training in the lab. Scholars interested in neuronal regeneration and repair will find the Duan lab a good fit.
Felice Dunn, PhD, Assistant Professor of Ophthalmology, is an NIH-funded investigator interested in understanding how visual information is parsed and processed in the retina, and how these functions are perturbed in disease. The lab focuses on the unique functional properties that make different types of bipolar cells suited to dividing a common photoreceptor input into distinct channels and how these bipolar cells react and remodel following damage to cones. Vision restoration following retinal disease requires a deeper understanding of how the retina processes information and how retinal circuits are damaged or reorganized during degeneration. Although still early in her career, Dr. Dunn has mentored several trainees who have garnered F32 fellowships and started their own research program at an outside institution. The Dunn lab will provide opportunities for Scholars interested in retinal circuit processing and photoreceptor degeneration.
Jacque Duncan, MD (Advisory Committee), Professor of Ophthalmology, leads an NIH-funded translational vision science laboratory focused on adaptive optics scanning laser ophthalmoscopy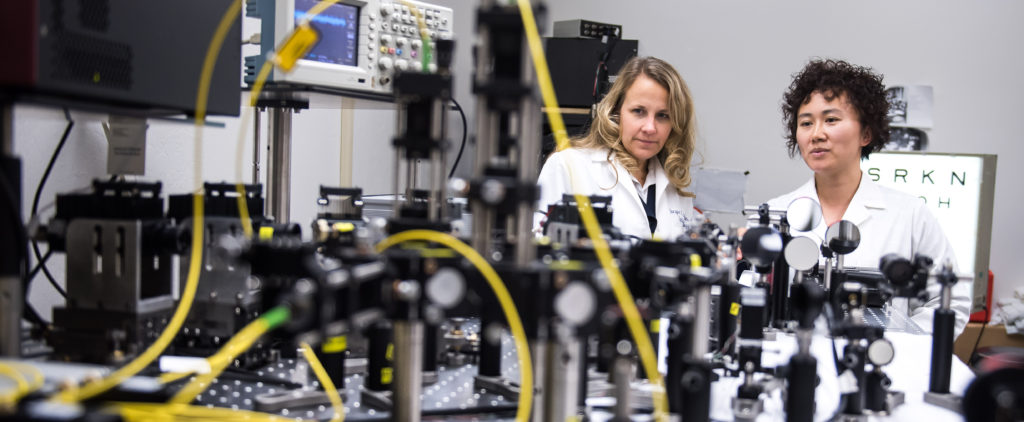 (AOSLO) imaging of human photoreceptors in order to discover mechanisms of cone death in various retinal degenerations. In addition, Dr. Duncan’s group is studying changes in cone structure and function during disease progression and testing the efficacy of treatments that aim to slow progression. Along with her collaborator Austin Roorda, PhD (UC Berkeley), they reported the first studies of cone structure during disease progression and in response to an experimental treatment. Dr. Duncan is also Co-PI on an Audacious Goals Initiatives proposal that will develop cone-dominant retinal disease models as a resource for translational vision research. Dr. Duncan’s group will characterize photoreceptor structure and function in patients with cone-rod dystrophy. In addition, Dr. Duncan is the study chair of a natural history study examining the rate of retinal degeneration due to mutations in the USH2a gene (the RUSH2A study), which has nearly completed enrollment at 20 retinal degeneration centers in the US and EU. Finally, Dr. Duncan has also received funding from the Foundation Fighting Blindness and the US Food and Drug Administration Office of Orphan Product Development to study the relationship between cone survival and treatment with ciliary neurotrophic factor. Dr. Duncan has longstanding interests in education, serving as Vice Chair for Medical Student Affairs in the Department of Ophthalmology and faculty mentor to the Ophthalmology Interest Group, and previously serving on the Integrated Curriculum Steering Committee and Medical Student Research Task Force. Scholars with an interest in translational vision sciences, retinal imaging, retinal degenerations, and medical education may identify Dr. Duncan as a Mentor.
(AOSLO) imaging of human photoreceptors in order to discover mechanisms of cone death in various retinal degenerations. In addition, Dr. Duncan’s group is studying changes in cone structure and function during disease progression and testing the efficacy of treatments that aim to slow progression. Along with her collaborator Austin Roorda, PhD (UC Berkeley), they reported the first studies of cone structure during disease progression and in response to an experimental treatment. Dr. Duncan is also Co-PI on an Audacious Goals Initiatives proposal that will develop cone-dominant retinal disease models as a resource for translational vision research. Dr. Duncan’s group will characterize photoreceptor structure and function in patients with cone-rod dystrophy. In addition, Dr. Duncan is the study chair of a natural history study examining the rate of retinal degeneration due to mutations in the USH2a gene (the RUSH2A study), which has nearly completed enrollment at 20 retinal degeneration centers in the US and EU. Finally, Dr. Duncan has also received funding from the Foundation Fighting Blindness and the US Food and Drug Administration Office of Orphan Product Development to study the relationship between cone survival and treatment with ciliary neurotrophic factor. Dr. Duncan has longstanding interests in education, serving as Vice Chair for Medical Student Affairs in the Department of Ophthalmology and faculty mentor to the Ophthalmology Interest Group, and previously serving on the Integrated Curriculum Steering Committee and Medical Student Research Task Force. Scholars with an interest in translational vision sciences, retinal imaging, retinal degenerations, and medical education may identify Dr. Duncan as a Mentor.
Douglas Gould, PhD (Advisory Committee), Director of Research and the Denise B. Evans Professor of Ophthalmology and Anatomy, is an NIH-funded investigator who uses genetic tools to study the role that extracellular matrix proteins play in human eye disease including glaucoma, retinal degenerations, and retinal neovascularization. His group also studies the role of ER stress in inherited retinal degenerations caused by protein misfolding and test preclinical therapeutic interventions to preserve photoreceptor survival and function. Dr. Gould also initiated the Department’s postdoctoral fellow training program, which entails identification of a co-mentor and semiannual mentoring meetings, a postdoc speaker series, and recognition and reward including an annual prize for the best vision science paper. In addition to the numerous postdoctoral fellows and graduate students Dr. Gould has mentored, he has also recently mentored two residents and will be the mentor for incoming clinician-scientist Tyson Kim, MD, PhD. The Gould lab will provide opportunities for Scholars interested in state-of-the-art genetic tools, extracellular matrix biology, and retinal degenerations.
Ari Green, MD, Associate Professor of Neurology, is the Division Chief of one of the largest research groups in the world dedicated to understanding multiple sclerosis (MS) and related disorders. The Green lab is particularly interested in developing means of harnessing glial biology to help repair damage to the CNS and in measuring this repair using vision-based metrics with an enhanced understanding of the visual system. The team has developed and optimized methods for performing visual evoked potentials and electroretinography in rodents and tools for determining the cellular and molecular basis of the signals detected. Finally, Dr. Green led the clinical translational team dedicated to the development of small molecules capable of remyelination and independently led the first successful clinical trial for remyelination in the setting of chronic injury in MS. Dr. Green has been a successful mentor, for example, two trainees receive their individual K awards under his mentorship. Scholars with an interest in translational vision sciences, visual system injury and repair, and clinical trials work may find the Green lab a good fit.
Jonathan Horton, MD, PhD, Professor of Ophthalmology, Neurology, and Physiology, is a neuro-ophthalmologist who studies the neural mechanisms underlying visual loss caused by amblyopia and strabismus. His NIH-funded laboratory studies alert, behaving primates to probe the physiologic basis of visual suppression, eye movements, and disorders of binocular vision. By employing cytochrome oxidase histochemistry as a measure of brain activity, the Horton lab has sought consistently to link function and structure. In recent years the lab’s focus has shifted direction, putting aside cortical anatomy, amblyopia, and acute, anesthetized physiology in favor of studies about strabismus in alert, behaving macaques or human patients. Dr. Horton’s laboratory research is often inspired and guided by the patients he encounters with visual problems in his clinic. He has mentored numerous graduate students, medical students, postdoctoral fellows, residents, and junior faculty members at UCSF. Scholars with an interest in disorders of binocular vision in non-human primates and human patients may find the Horton lab a good fit.
Aparna Lakkaraju, PhD, Associate Professor of Ophthalmology, is interested in  translational retinal cell biology, with particular emphasis on retinal pigment epithelial cell physiology. Her NIH-funded work investigates mechanisms that regulate critical processes including cellular debris clearance, mitochondrial dynamics, RPE-photoreceptor communication, drusen biogenesis, and ocular immune privilege. As a mentor, Dr. Lakkaraju has committed time to several STEM outreach activities, including Expanding Your Horizons conference for middle school girls. She has also served as a faculty mentor in the Women in Science and Engineering (UW Madison) and Women’s Leadership Development program (Association for Research in Vision and Ophthalmology).
translational retinal cell biology, with particular emphasis on retinal pigment epithelial cell physiology. Her NIH-funded work investigates mechanisms that regulate critical processes including cellular debris clearance, mitochondrial dynamics, RPE-photoreceptor communication, drusen biogenesis, and ocular immune privilege. As a mentor, Dr. Lakkaraju has committed time to several STEM outreach activities, including Expanding Your Horizons conference for middle school girls. She has also served as a faculty mentor in the Women in Science and Engineering (UW Madison) and Women’s Leadership Development program (Association for Research in Vision and Ophthalmology).
Sarah Knox, PhD, Associate Professor in the Department of Cell and Tissue Biology, runs an NEI-funded lab focused on nerve-epithelial communication and how this regulates organ development, regeneration, and autoimmune diseases such as Sjögren’s syndrome. Her lab has uncovered the link between chronic inflammation in Sjögren’s syndrometo nerve loss in the cornea and lacrimal gland. However, while current therapies do not address the need to maintain and/or reinnervate ocular tissues or stimulate tear secretion, the Knox lab is determining the neuroregenerative potential of a lacripep, a novel therapeutic for restoring innervation and tear secretion dry eye. Dr. Knox has mentored 8 postdocs, 8 graduate students, and 27 predoctoral students, including 6 URM, 1 disabled, and 4 LGBTQI trainees. Scholars interested in understanding neuroinflammation and regeneration will find opportunities in the Knox lab.
Deepak Lamba, MBBS, PhD, Associate Professor of Ophthalmology, leads an NIH-funded laboratory focused on retinal repair following inherited and age-associated degeneration and utilizing stem cells to generate disease-in-a-dish models. He was one of the first in the US to publish his retinal differentiation protocols and use them for regenerative medicine. Dr. Lamba is a natural collaborator with clinician-scientists and since joining the Department in 2018 he has established collaborations with Drs. Jacque Duncan and Tony Moore. Dr. Lamba has mentored numerous pre- and postdoctorates and is also a member of the resident research committee. His group will provide opportunities for Scholars interested in harnessing the power of novel stem cell technologies to clinical problems especially retinal degenerations.
Anthony Moore, MD, Professor of Ophthalmology, is a world expert in ophthalmic genetics and his team is focused on identifying the genes causing childhood onset retinal dystrophies utilizing next generation sequencing techniques and carrying out detailed phenotyping of patients where causative mutations are identified. Dr. Moore is also interested in developing new therapies for these blinding disorders. With Dr. Anne Slavotinek in Clinical Genetics at UCSF, the Moore group is identifying novel genes causing developmental eye disorders. Dr. Moore also leads a collaboration with Dr. Bruce Conklin at the Gladstone Institute using CRISPR technology to treat inherited retinal degenerations. With Dr. Doug Gould and UCSF ophthalmology resident Dr. Lesley Everett, the team is studying two rare recessive human disorders where there is a complete lack of development of retinal vessels. Using mouse models, the team is examining the biological pathway involved, which may be distinct from VEGF and thus may be a novel target for inhibiting retinal neovascularization. Finally, Dr. Moore is the local PI of an ocular gene therapy trial for Juvenile X-linked retinoschisis sponsored by AGTC. UCSF is one of seven centers nationally taking part in this multicenter Phase 1/2 study. Dr. Moore has mentored numerous pre- and postdoctorates, residents, and fellows, as well as junior faculty members. The Moore group will provide opportunities for Scholars interested in inherited retinal degenerations, ocular genetics and therapeutics, and translational vision science.
Maxence Nachury, PhD, Associate Professor of Ophthalmology, is an NIH-funded investigator interested in the fundamental question of how trafficking influences signaling decisions made at the primary cilium. His lab is focused on understanding the molecular activity of the more than 20 gene products whose dysfunction causes Bardet-Biedl Syndrome (BBS), a prototypical ciliopathy characterized by retinal degeneration, obesity, polydactyly, and polycystic kidneys. The Nachury lab uses inputs from human genetics, mouse models, cell biology, biochemistry, biophysics, and structural biology. Of the twelve postdoctoral fellows and one graduate student Dr. Nachury has mentored, nearly twenty successful fellowship applications resulted and nearly half of the postdoctoral fellows trained have or have been offered faculty positions. The Nachury lab will provide opportunities for Scholars interested in the cell biology underlying retinal degenerations.
Sai Nair, PhD, Assistant Professor of Ophthalmology, uses mouse genetics to understand mechanisms of glaucoma and ocular growth. His lab is developing mouse models that reflect the genetic complexity of glaucoma and myopia. The Nair lab has identified specific mutations in mice that cause phenotypes that model key features of human angle closure glaucoma and employs comparative genomics to assess molecular pathways that can be targeted for therapeutic intervention in glaucoma. Dr. Nair is committed to mentoring undergraduates, postdoctoral fellows, and other researchers, and his trainees have done well in terms of high-profile publications and competing for individual fellowships. The Nair lab will provide opportunities for Scholars interested in ocular genetics and comparative genomics.
Yvonne Ou, MD (Co-PI/Co-PD), Associate Professor of Ophthalmology, leads an NIH-funded laboratory that is examining the circuitry of the inner retina and its potential for plasticity in glaucoma. Her K08 mentored research training with Drs. Erik Ullian and David Sretavan was focused on the compartmentalized neurodegeneration of the retinal ganglion cell in glaucoma. Recent work has centered on the cellular and synaptic mechanisms of ganglion cell degeneration and identifying specific types of ganglion cells and circuits that are particularly susceptible in glaucoma. As a clinician-scientist, Dr. Ou is not only motivated to advance the field by answering these fundamental questions, but also by translating the knowledge into improvements in diagnostic modalities using novel visual field and ERG stimuli. In addition to serving as Co-Director of the Glaucoma service, Dr. Ou is also the Department of Ophthalmology’s Vice Chair for Postgraduate Education, actively involved in the academic and career development of clinical and research fellows. Scholars interested in retinal circuitry, neurodegeneration, and translational studies would find the Ou lab a good fit.
Michael Stryker, PhD, Professor in the Department of Physiology and former Chair of Physiology at UCSF, is a world-renowned neuroscientist interested in the mechanisms underlying development and plasticity of precise connections within the central nervous system, specifically the visual system. The approaches used by the Stryker laboratory include manipulations of visual experience, electrophysiology in vivo, modern optical imaging and microscopy, computer vision models, pharmacology, and genetic and anatomical techniques. Dr. Stryker is very committed to excellence in teaching and mentoring at both the graduate and postdoctoral level, as evidenced by the fact that 75% of his trainees have become tenured or tenure-track at top-notch research institutions. He also regularly teaches in the UCSF course on ethics and responsible research. Scholars with an interest in the neural circuit substrates of adult plasticity and the visual system may find the Stryker lab a good fit.
Erik Ullian, PhD, Professor of Ophthalmology, studies molecular mechanisms that regulate synapse formation and function in the visual system. He has used cell culture systems to screen for genes and small RNAs that impact synaptic transmission. His laboratory has identified the miRNA pathway as an important regulator of a variety of neuronal and synaptic processes relevant to visual system development. The Ullian lab is also studying the interactions between neurons and glia that are required for proper development and function of the nervous system. He is developing astrocyte, neuron, and microglial 3D organoids to model key aspects of neurodegenerative diseases. In addition to graduate students and postdoctoral fellows, Dr. Ullian has mentored K awardees, including Dr. Yvonne Ou. Scholars who are interested in the interactions of neurons and glia in the visual system will be interested in the Ullian lab.
The Department has a robust program dedicated to applying bioengineering principles and innovative solutions for unmet clinical needs in ophthalmology. For example, through close collaborations with the Department of Bioengineering & Therapeutic Sciences at UCSF, scientists at Caltech, and the innovation team at QB3 (California Institute for Biosciences), Department of Ophthalmology faculty have developed innovative devices and technologies to improve drug delivery, surgical devices, and retinal imaging. Faculty
Mentors on this Track include:
Robert Bhisitkul, MD, PhD, Professor of Ophthalmology and Director of the Retina Fellowship, is a vitreoretinal specialist who in collaboration with UCSF’s bioengineering group has developed a novel thin-film drug delivery system that can produce long term zero order kinetics through regulating pore sizes at nanoscale. This is now being tested in vivo for delivery of anti-VEGF agents. In addition to his bioengineering projects, he directed the SEVEN-UP cohort study of long-term outcomes in age-related macular degeneration treatment and is an investigator in major clinical trials of new retinal therapies. As Director of the Retina Fellowship, Dr. Bhisitkul has mentored many clinical fellows as well as research fellows. Scholars interested in ocular drug delivery and clinical trials will be interested in the Bhisitkul lab.
Ying Han, MD, PhD, Associate Professor of Ophthalmology, Co-Director of the Glaucoma service, and Glaucoma Fellowship Director, is a glaucoma specialist whose research addresses the need for improved and fibrosis-free surgical implants for glaucoma. In collaboration with bioengineers and material sciences, she leads NIH-funded work developing novel microfluidic meshworks for use in glaucoma drainage implants. In addition, she has organized a multicenter international RCT to examine the role of intra- and postoperative mitomycin-C for use with Ahmed glaucoma valves. Other projects include integrated wireless microactuators for fibrosis control in glaucoma drainage devices and microfluidic contact lens sensors for intraocular pressure monitoring. Dr. Han as mentored many pre- and postdoctorates, as well as clinical and research fellows. Scholars interested in tackling unmet surgical needs in ophthalmology may identify Dr. Han as a Mentor.
Stephen McLeod, MD (Chair of the Advisory Committee), the Theresa M. and Wayne M. Caygill, MD, Distinguished Professor and Chair of the Department of Ophthalmology, is interested in the development of implanted accommodating devices and new devices in cataract surgery. He also collaborates with colleagues at the Proctor Foundation in studies of the optimal treatment of infectious keratitis worldwide. Dr. McLeod is Editor-in-Chief of Ophthalmology, serves on the board of directors for the American Board of Ophthalmology and the Heed Ophthalmic Foundation, and is a member of the Ophthalmic Devices Panel of the Medical Devices Advisory Committee of the FDA and the National Advisory Eye Council of the NIH. As Chair of the Department, Dr. McLeod has mentored and developed the clinician-scientist careers of many faculty. He is also actively involved in resident education, including serving on the Board of Directors for the Heed Foundation. Scholars with an interest in ophthalmic device development will identify Dr. McLeod as a Mentor.
Daniel Schwartz, MD (Advisory Committee), Professor of Ophthalmology and Director of the Retina service, is a vitreoretinal surgeon whose research has focused on the development devices and technologies that address unmet needs in ophthalmology. In collaboration with Caltech, he co-invented and helped develop a light-adjustable intraocular lens material that can be used to calibrate residual refractive error after cataract surgery (FDA approvedin 2017) He also co-invented and helped develop OCT angiography as a non-invasive and superior alternative to fluorescein angiography. Current work includes the development of light adjustable materials that can be used to modify scleral biomechanics so as to retard myopia development. Dr. Schwartz has mentored many medical students, residents, and fellows, and has provided research mentorship to over 18 postdoctoral fellows. Scholars who are interested in tackling unmet ophthalmology clinical needs by rapidly developing technologies may identify Dr. Schwartz as a Mentor.
Jay Stewart, MD, Professor of Ophthalmology and Chief of Ophthalmology at San Francisco General Hospital, leads an NIH-funded research program focused on drug delivery and assessing the safety and efficacy of ultrasound technologies that can promote corneal and transscleral penetration of topical agents. The lab is also interested in evaluating the mechanisms determining biomechanical properties and stiffness of ocular tissues. This work spans therapeutic interventions such as corneal cross-linking and pathologic processes such as diabetic retinopathy and vitreopathy. Dr. Stewart is also conducting a prospective clinical trial to assess the effect of metformin use on age-related macular degeneration and progression to choroidal neovascularization or geographic atrophy. He has mentored numerous pre- and postdoctorates, as well as two junior faculty members. The Stewart lab will provide opportunities for Scholars interested in drug delivery and ocular biomechanics.