Just Getting Started: $2.5 Million for Mentorships
UCSF Ophthalmology’s outstanding vision and clinician scientists have a tremendous track record of developing leading-edge research programs that attract hypercompetitive grants from the National Institutes of Health (NIH). This sustained funding enables new discoveries
 The UCSF-Proctor Clinician Vision Scholars K12 Program is a $2.5 million, five-year grant from the National Eye Institute (NEI), one of 27 institutes and centers that comprise the US National Institutes of Health. This grant provides institutional funding to train as many as ten young faculty members to achieve this same level of success. Co-led by Yvonne Ou, MD, and Tom Lietman, MD – both NEI grant awardees – the program builds on existing strengths and collaborations in clinical and translational sciences, bioengineering, and career development in the UCSF Proctor Foundation and Department of Ophthalmology.
The UCSF-Proctor Clinician Vision Scholars K12 Program is a $2.5 million, five-year grant from the National Eye Institute (NEI), one of 27 institutes and centers that comprise the US National Institutes of Health. This grant provides institutional funding to train as many as ten young faculty members to achieve this same level of success. Co-led by Yvonne Ou, MD, and Tom Lietman, MD – both NEI grant awardees – the program builds on existing strengths and collaborations in clinical and translational sciences, bioengineering, and career development in the UCSF Proctor Foundation and Department of Ophthalmology.
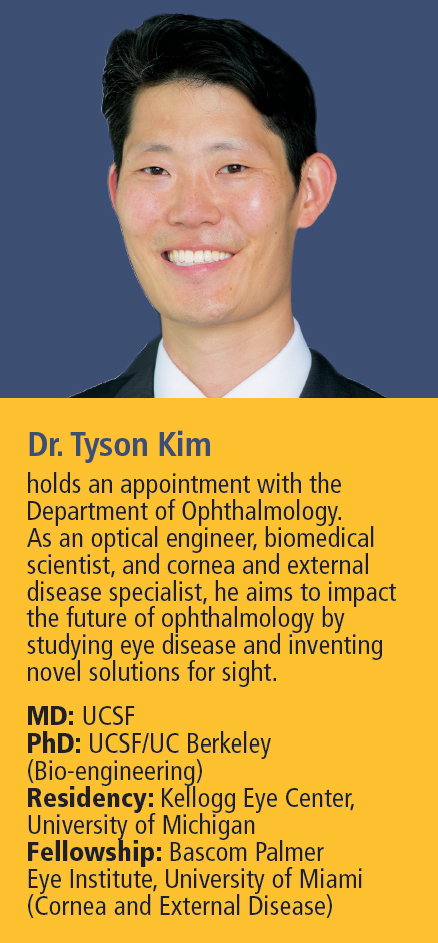
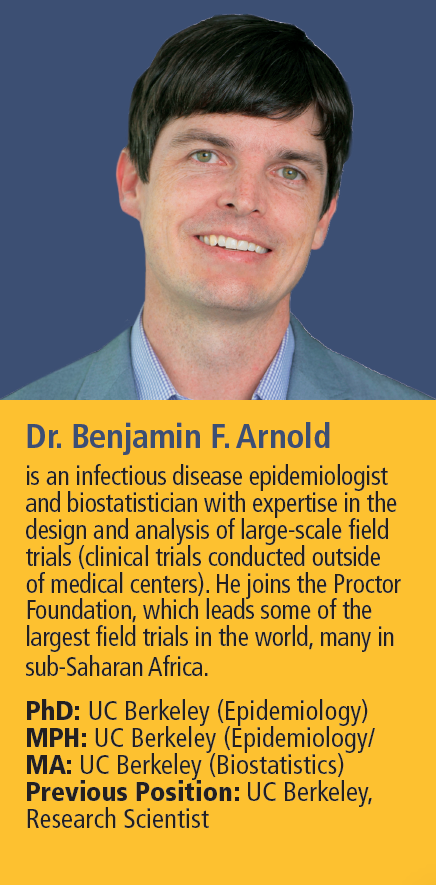
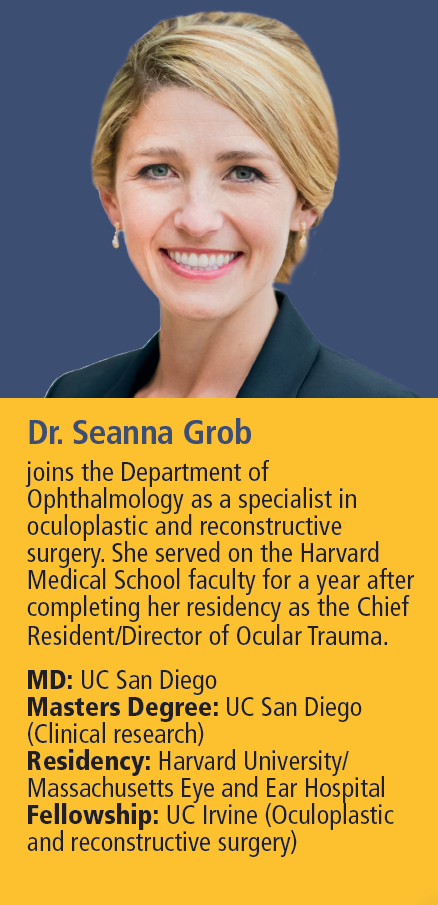
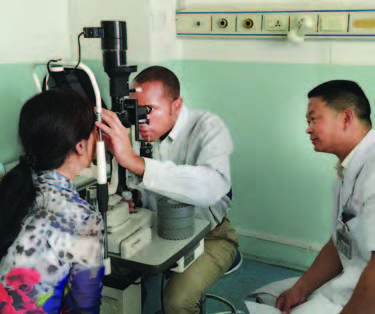
New patient-serving faculty members with a passion for research can undertake a one-year intensive mentorship, each supported by a primary mentor and a faculty advisory committee. Immersion in rigorous state-of-the-art vision research is supplemented with guidance for crafting important and novel questions while developing techniques to answer them, aspects of leadership, the value of multidisciplinary and collaborative approaches, and writing effective grant proposals.
This mentorship opportunity makes UCSF Ophthalmology an even more attractive place for top clinical research candidates to launch their faculty careers. As younger vision scientists develop and take charge of significant new research programs, the future of vision grows brighter – at UCSF and around the world.
Reducing Sight Loss from Diabetes
Cathy Sun, MD, the first scholar to benefit from an NEI K12 mentorship, has been awarded an NIH grant for independent research of diabetic retinopathy.

Joining UCSF Ophthalmology’s faculty in 2019, Dr. Sun’s grant will allow her to investigate the rising global health threat of Type 2 diabetes, where blurred vision is often the first noticeable symptom. Advanced diabetic eye disease, called proliferative diabetic retinopathy, can result in permanent sight loss.
Dr. Sun and her team develop and test novel methods and tools for analyzing large databases of de-identified electronic health care records of patients treated for this condition. The team’s findings and insights can be used to adjust treatment protocols, halting the disorder before it advances and reducing sight loss. They expect to improve strategies for electronic records investigations that can be used to improve outcomes for other damaging eye conditions as well.
Dr. Sun earned her medical degree and completed a residency in ophthalmology at UCSF. She completed a fellowship in glaucoma at Bascom Palmer Eye Institute and received a merit award fellowship from the prestigious Heed Ophthalmic Foundation.