Telemedicine: The use of technology to connect patients and healthcare providers who cannot interact in person.
The concept of today’s telemedicine goes back to the 1950s. Originally used to link rural patients with medical staff in more centralized locations, the COVID-19 pandemic of 2020 has brought the clinic into everyone’s home. But even before sheltering-in-place, UCSF doctors have been using and refining telemedicine from the Tenderloin to Thailand. (Photo caption: Using a special attachment, a field technician turns his smartphone into an optical camera.)
San Francisco: Diabetes and Glaucoma Mobile Screenings
The prevalence of diabetes is growing, both in the United States and worldwide. As a result, the frequency of diabetic retinopathy (DR) and vision threatening diabetic retinopathy (VTDR) is also expected to increase dramatically. Individuals with Type 1 diabetes should have annual screenings for DR beginning five years after the onset of their disease. Those with Type 2 diabetes need a prompt examination at the time of diagnosis and at least yearly examinations thereafter. However, only about 60% of those with either form of diabetes currently have yearly screenings.

Enter the Eye Van
Gifts from the Friends of the Congressional Glaucoma Caucus Foundation, the San Francisco Health Plan, and That Man May See allowed purchase of a van in 2004 that is used by a collaboration of UCSF, San Francisco General Hospital (now Zuckerberg San Francisco General Hospital or ZSFGH), and the San Francisco Community Health Network (CHN). This van provides mobile eye care as well as glaucoma and retinal screenings for San Francisco’s underserved population.
With funding from the city and county of San Francisco, grants from the state of California, UCSF, and ZSFGH, and the teamwork of UCSF Retina faculty Armin Afshar, MD, MBA, Director of Tele-Ophthalmology for the San Francisco Department of Public Health, and Jay Stewart, MD, Chief of Ophthalmology at ZSFGH, the 28-foot Eye Van was refurbished in 2017. This allowed a state-of-the-art ultra-widefield fundus camera to be mounted inside. This camera captures images of the back portion of the eye: the retina, macula, fovea, optic disc, and posterior pole.
How It Works
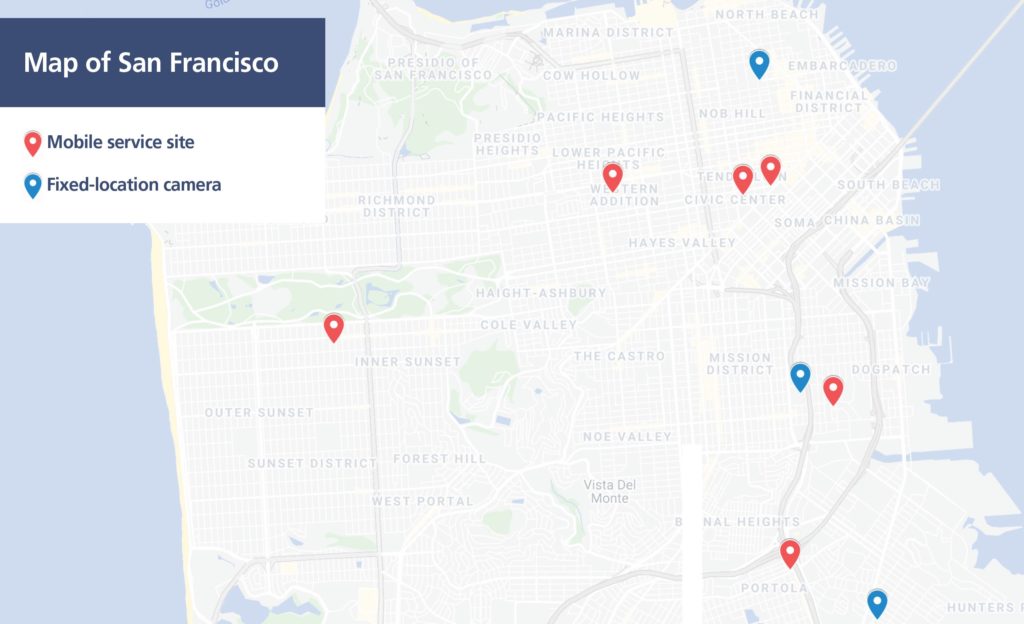
With a technician, the Eye Van is sent on a rotational schedule to primary care clinics in areas of need throughout San Francisco. Additional retinal cameras in four community health center primary clinic locations in the city allow patients to receive diabetic retinal screenings at the same time and location as their physician visits.
Dubbed the “ZSFGH Eye Clinic on Wheels,” the van connects to Wi-Fi at each primary care health center as it arrives. The patient’s electronic health record is accessible from an on-board computer and demographic/clinical information is collected at the time of the screening.
Retinal images are taken without the need for dilating eye drops, then uploaded wirelessly to the server. These photographs are transmitted to a reading center at ZSFGH where they are graded by trained readers for diabetic retinopathy (DR) and other sight-threatening diseases, such as glaucoma and cataracts. If potential eye issues are identified, the patient is referred to the ZSFGH ophthalmology clinic.
Analyzing the Impact
In an article published in Ophthalmology Retina in 2019, the Proctor Foundation’s Catherine Oldenburg, ScD, MPH, joined Drs. Afshar and Stewart in reporting on initial results of the ZSFGH tele-retinal screening program. A total of 2,788 patients were screened in the diverse urban population of San Francisco, which included the underserved, the disabled, the homeless, and the prison population.
Beyond the Eye Van
A $51,000 UCSF President’s Innovation Fund Award to optimize screening for pediatric diabetic retinopathy with a telemedicine screening program was given to Pediatric Endocrinology Fellow Fatema Abdulhussein, MD, in collaboration with UCSF Pediatric Ophthalmology Director Alejandra de Alba Campomanes, MD, MPH, resident Murtaza Saifee, MD, and Dr. Afshar.
The award covers the purchase of an ultra-widefield retinal camera for the UCSF Madison Pediatric Diabetes Clinic at Mission Bay, so that children with the disease can conveniently have retinal photographs taken during their endocrinology visits. These images are then transmitted to UCSF ophthalmology faculty for screening for diabetic eye disease.
Thailand: Diagnosis Beyond the Clinic

In the city of Chiang Mai, Thailand, Francis I. Proctor Foundation’s Jeremy Keenan, MD, MPH, researched the use of telemedicine for diagnosing cytomegalovirus (CMV) retinitis, a potentially blinding complication from acquired immunodeficiency syndrome (AIDS). Because people are unlikely to see an ophthalmologist before vision loss has already begun to occur, CMV retinitis is often not caught at an early phase.
Telemedicine is now providing far more opportunities to save vision. Portable retinal cameras capture an image of a patient’s eyes and are sent electronically to remote retinal specialists to determine whether there is development of CMV retinitis. In Thailand, ophthalmologists and health care providers are a scarce resource, so being able to prioritize their time by having non-medical photographers assist with the detection process makes a huge impact. Additionally, this expands the number of individuals who can be screened since the photographer can easily travel to take the photos.
Ever Improving
Dr. Keenan is working with Daniel Fletcher, PhD, of UC Berkeley, and Todd Margolis, MD, PhD, of Washington University, to develop an attachment to convert a smartphone into a retinal camera and anterior segment camera, offering a cost-effective approach to screening in resource-limited settings. Masters students in the Berkeley bioengineering program have been vital to this project. Supporting more students to work with the team is the next step in the process of creating an improved telemedicine option.
A Broader Impact
The COVID-19 pandemic has highlighted the need for telemedicine like never before, and it is especially important in areas like Thailand, where medical resources can be sparse. As Dr. Keenan’s team is currently engaged in more hospital-based work, the goal is to include more community-based service. The addition of another retinal camera will allow for more diagnoses to be made while the handheld retinal camera is still in development.
With initial seed funding from That Man May See, the impact of research like Dr. Keenan’s has given a second chance at sight for those who might not have otherwise been diagnosed in time.
Looking Forward
Telemedicine makes it easier for patients to receive high-quality ophthalmic care regardless of their location. It also enables health care providers to offer services to broader, more diverse patient populations. The future will bring patient and provider closer together, no matter how far apart geographically.

