The Nair Lab
Studying the genetics and biology of ocular diseases
Our Research
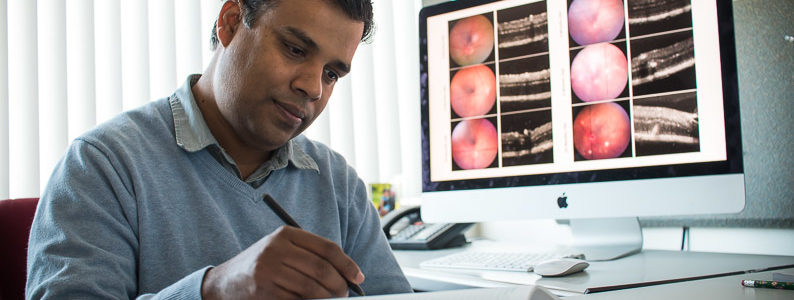
The main goal of our laboratory is to identify and characterize genetic factors contributing to ocular diseases with a major focus on glaucoma. Glaucoma is a group of diseases that leads to progressive degeneration of the optic nerve and loss of retinal ganglion cell (RGC) bodies in the retina. It is a leading cause of irreversible blindness. The current knowledge on glaucoma causing genes is limited. This is mainly because glaucoma is primarily a complex multigenic disease. This makes it challenging to identify glaucoma relevant genes and prove their direct involvement in disease causation. To help determine these genetic factors, we utilize various murine models that serve as a powerful tool to identify/validate glaucoma causing genes and provide mechanistic insights into disease pathogenesis.
Our studies integrate two complementary approaches. In the first approach, we investigate how various human candidate genes/pathways (emerging from human linkage or genome-wide association studies) contribute to glaucoma relevant conditions using the mouse. This is mainly achieved by creating genetically modified mice in which the mouse equivalent of the implicated human gene is altered. In a complementary yet synergistic approach, findings from our mouse models of glaucoma are extrapolated to understanding the human disease. Mouse genetics driven experiments along with gene expression analysis in established murine glaucoma models are used to gain insight into the genes/pathways contributing to high intraocular pressure (IOP, a major risk factor for glaucoma) and glaucomatous neurodegeneration. Thereafter, the relevance of the data obtained in mice is extended to human glaucoma by using tools of comparative genetics/genomics.
Our experience in employing the mouse to dissect complex genetic diseases puts us in a unique position to identify and functionally elucidate the role of glaucoma causing genes at a mechanistic level. We utilize a multi-disciplinary approach by integrating the use of genetics, genomics, molecular biology, cell-biology and physiology based experiments in our research.
The various ongoing projects:
1. Molecular Mechanisms Contributing to Elevated Intraocular Pressure and Glaucoma
With an aging population, glaucoma, which leads to irreversible blindness, is a major public health concern impacting 2.7 million people in the US alone and the burden is expected to top 7.3 million by the year 2050. Elevated intraocular pressure (IOP) due to impaired aqueous humor drainage caused by dysfunctional ocular drainage tissues is a major risk factor of glaucoma. Despite its severity, little is known about the causal genes regulating high IOP and glaucoma. There is an urgent need to develop early biomarkers of the disease and identify therapeutic gene targets. have recently identified Krüppel-like zinc finger transcriptional factor GLIS1, as a regulator of trabecular meshwork (TM, key component of ocular drainage structure) structure and function as well as maintenance of normal IOP. Supporting this finding we showed that GLIS1 is predominantly expressed in the TM and its deficiency in mice leads to progressive degeneration of the TM, resulting in inefficient AqH drainage and elevated IOP. Furthermore, we and others have found an association between variants of GLIS1and primary open angle glaucoma (POAG) making our finding relevant to human patients3. To our knowledge, GLIS1 is the first transcription factor experimentally demonstrated as necessary for maintaining TM structure and function. Building on these key findings, the aim of this proposal is to define a role for GLIS1 dependent transcriptional program in maintenance of the ocular drainage tissue form and function. In parallel, we are testing the role of some for the genes identified through our GWAS analysis that are predicted to induce glaucoma through their effect on retina/optic nerve by developing genetic mouse models lacking the specific gene of interest.
Overall, our study is aimed at characterizing novel and unique preclinical models of human glaucoma and will aid the discovery of novel disease biomarkers and targets genes to inform therapeutic intervention strategies to treat or ameliorate high IOP and POAG.
2. Functional Characterization of Human Glaucoma Loci
We have combined human genetics and mouse models to gain mechanistic insight into genetics factors contributing to high IOP and glaucomatous neurodegeneration. Our experiments are aimed at a) Identifying gene regulatory elements in glaucoma-relevant IOP loci in human trabecular meshwork (TM) cells, b) Determining which genetic variants in these elements alter regulatory function, c) Determining the consequences of these changes on the function of ocular drainage tissues and IOP. To do this, we are conducting ATAC-seq and ChIP-seq in primary human TM cells to identify potential gene regulatory elements. We will characterize the effect of IOP loci on gene regulatory element function and determine how these regulatory changes contribute to ocular drainage tissue specific defects and elevated IOP. A similar approach for characterizing genetic loci that are predicted to act through retinal cell-types and likely contributing to glaucomatous neurodegeneration will be subsequently conducted.
3. Molecular Players Contributing to Ocular Refractive Development and Myopia
Refractive errors are a major cause of vision loss worldwide, and the rising prevalence of myopia and associated blinding conditions is a significant public health concern. Regulation of ocular axial growth is critical for normal refractive development to ensure that a focused image falls directly on the retina. Our goal is to decode the molecular and genetic program that governs ocular axial growth and refractive development. We have identified PRSS56 (secreted serine protease) as a molecule that regulates ocular axial growth and is essential for proper refractive development of the eye. Utilizing genetic mouse models, we have demonstrated that the loss of PRSS56 function causes a decrease in ocular axial length and its increased activity causes ocular axial elongation.
Multiple lines of evidence suggest a key role for PRSS56 in myopia pathogenesis: a) GWAS from several groups have found an association between PRSS56 variants and myopia, b) Recent studies have found upregulation of Prss56 mRNA levels in marmoset retina in response to lens-induced (optical defocus dependent) axial elongation. Despite evidence that altered expression of PRSS56 affects ocular axial length, the factors that regulate its expression and mediate its effect are not known. 1) Our research is focused on identifying upstream effector and downstream mediators of PRSS56 function. 2) Employing proteomics based approaches we are characterizing the function of PRSS56 protease that will guide the identification of its substrate(s) and targeted therapies. We are assessing small molecules with potential to inhibit PRSS56 activity and prevent or slowdown axial elongation (aimed at inhibiting serine protease activity). 3) Finally, we are testing the role of PRSS56 in vision guided ocular growth by temporarily inactivating PRSS56 in conditional mutant mice and using experimental paradigms that induce axial elongation in response to visual blur or optical defocus.